Associação Portuguesa de Investigação em Cancro
Do bloco ao laboratório: a visão do patologista sobre organóides tubo-ováricos
Do bloco ao laboratório: a visão do patologista sobre organóides tubo-ováricos
O carcinoma tubo-ovárico constitui uma das principais causas de mortalidade ginecológica e carece de modelos pré-clínicos que reproduzam de forma fidedigna a sua heterogeneidade biológica. Neste estudo, resultado da colaboração entre o Gulbenkian Institute of Molecular Medicine e o Hospital CUF Descobertas, foram estabelecidos organóides derivados de doentes, a partir de carcinomas serosos de alto e baixo grau, e de trompa de Falópio normal, preservando as características morfológicas e imunofenotípicas dos tecidos de origem. Estes resultados evidenciam o potencial dos organóides como modelos experimentais para a investigação da biologia tumoral e para a avaliação de estratégias terapêuticas. O trabalho reforça ainda o papel central do patologista na colheita das amostras e caracterização dos organóides, sublinhando a relevância da colaboração multidisciplinar no desenvolvimento de modelos in vitro com aplicabilidade clínica.
Autores e afiliações:
Catarina Alves-Vale1,2,3,4*, Beatriz Galvão2*, Ana Rita Silvestre1, José Silva Pereira4, Li Bei4, João Paulo Fernandes4, Paula Borralho1,3, Maria Carmo-Fonseca 2,3, Noélia Custódio2,3
1 – Department of Pathology, CUF Oncologia, Lisboa, Portugal
2 – Gulbenkian Institute for Molecular Medicine, Lisboa, Portugal
3 – Faculdade de Medicina, Universidade de Lisboa, Lisboa, Portugal
4 – Gynaecological Oncology Unit, CUF Oncologia, Lisboa, Portugal
*These authors equally contributed to this paper.
Abstract:
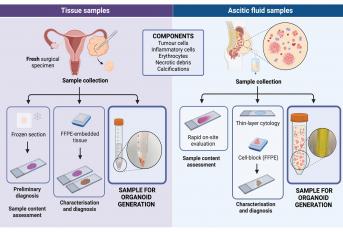
Tubo-ovarian carcinoma, a leading cause of gynaecological-related mortality, holds substantial biological and clinical heterogeneity. Despite advancements in drug development, predicting therapeutic efficacy remains challenging, partly due to the limited availability of in vitro models that accurately replicate tumour behaviour. We present a concise overview of the intrahospital workflow for establishing patient-derived organoids and analyse the morphological and immunophenotypical features of high-grade serous carcinoma (HGSC), serous borderline tumour (SBT)/low-grade serous carcinoma (LGSC), and normal fallopian tube (FT) organoids.
Samples were collected from patients undergoing surgery or paracentesis. Tissue underwent mechanical and enzymatical digestion. Resulting cell suspensions were resuspended in an extracellular matrix substitute for subsequent culture. Despite the low efficacy in establishing HGSC organoids (n = 1/7, 14%; 96 days, 11 passages), we successfully established two organoid lines of SBT/LGSC (n = 2/2, 100%; 65 days, 7 passages; 134 days, 16 passages) and normal FT (n = 2/2, 100%; 73 days, 10 passages; 58 days, 8 passages). HGSC organoids exhibited limited growth and mostly irregular structures, while preserving the p53 immunostaining pattern of the original tumour. SBT/LGSC and FT organoids maintained features of architectural complexity and faithfully recapitulated the original immunoprofile.
This study highlights the need for a multidisciplinary collaboration in both clinical and research settings to establish patient-derived organoids. It emphasises the pivotal contribution of pathologists in meticulous sampling and organoid characterisation. The integration of diverse expertise is essential for maximising the potential of organoids as preclinical tools, advancing our understanding of tubo-ovarian carcinoma, and ultimately improving patient outcomes.
Revista: Journal of Ovarian Research
Link: https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01766-4




